The Silent Assassin: Why Cardiovascular Disease Is The World’s Leading Disease
It does not have the cinematic terror of a pandemic virus or the sudden violence of a natural disaster. It operates in the quiet hum of daily life—in the traffic jam on your commute, in the processed lunch at your desk, and in the microscopic particles of the air you breathe.
Cardiovascular Disease (CVD) is the undisputed apex predator of human health. According to the latest global data released in late 2024, CVD now claims an estimated 19.8 million lives annually. To put that in perspective, that is roughly equivalent to the entire population of New York State vanishing every single year. It kills more people than all forms of cancer combined.
For decades, the narrative around heart disease has been simple: “Eat less fat, exercise more.” But as we move through 2025, science is revealing a far more complex and disturbing picture. This is not just a disease of aging or gluttony; it is a systemic failure driven by environmental toxins, genetic ghosts, and the invisible stress of modern existence.
The Anatomy of Silence: Why We Don’t See It Coming
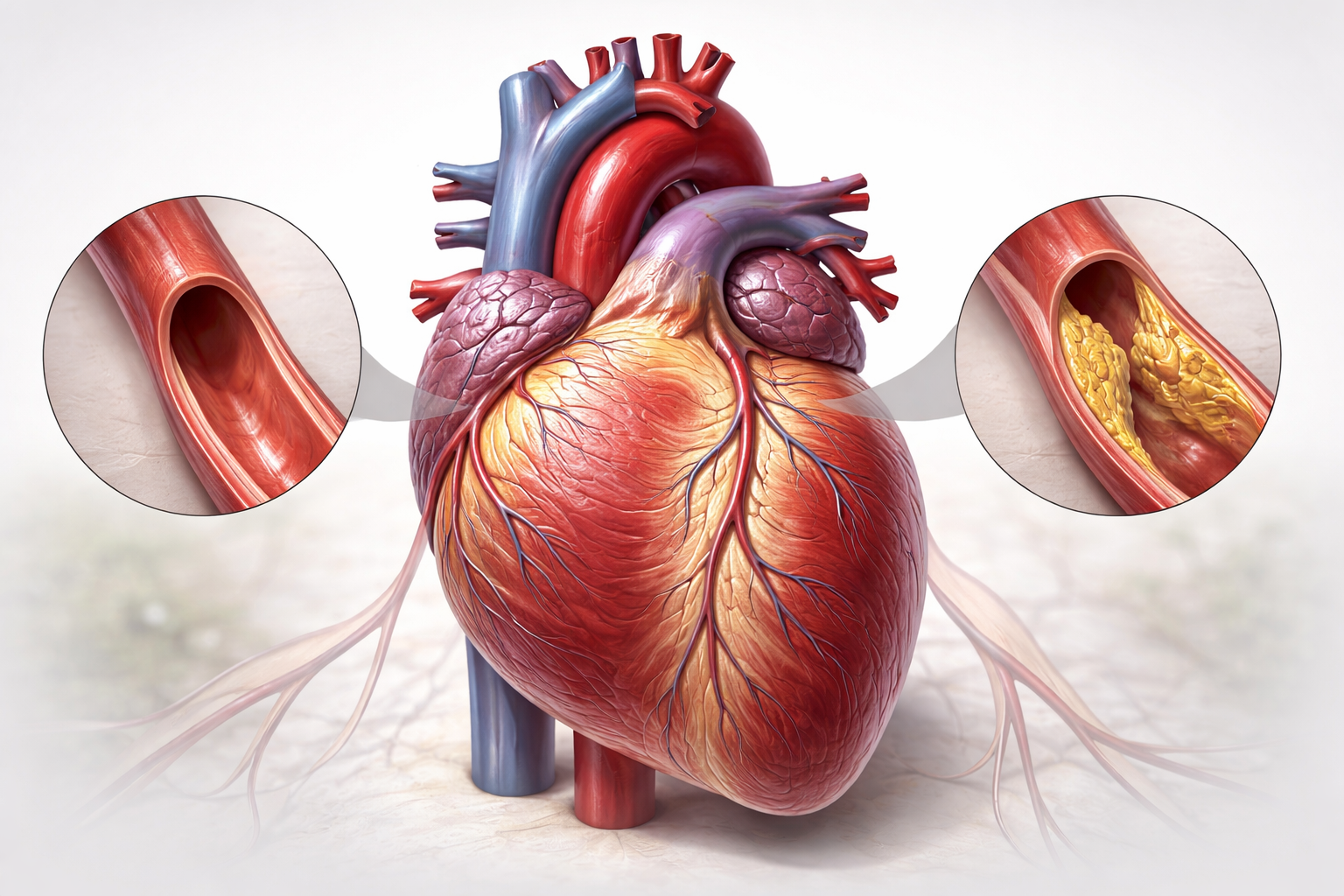
The most terrifying aspect of CVD is its stealth. The condition is often asymptomatic for decades. Atherosclerosis—the hardening and narrowing of arteries—begins not at age 50, but often in childhood.
Fatty streaks have been found in the aortas of children as young as 10. Over years, this soft plaque calcifies, narrowing the highways of blood that feed the brain and heart. The body is remarkably adaptable; it can function with arteries that are 70% blocked without a single symptom. The first symptom for over 50% of men and 64% of women who die of ischemic heart disease is the fatal heart attack itself.
This “silence” is why CVD remains the world’s leading killer. We treat it only when the catastrophe happens, ignoring the fire that has been smoldering for thirty years.
The “Uncommon” Drivers: What Your Doctor Might Not Check
Standard medical checkups focus on the “Big Five”: smoking, diabetes, hypertension, obesity, and LDL cholesterol. While critical, these factors fail to explain why nearly 50% of heart attack victims have normal cholesterol levels.
The cutting edge of cardiology in 2025 is focused on the “uncommon” drivers—the hidden variables that are fueling the modern epidemic.
- The Plastic in Your Veins (Microplastics)
In a landmark 2024 study published in The New England Journal of Medicine, researchers found a chilling link between pollution and plaque. They analyzed the arterial plaque of patients undergoing surgery and found microplastics and nanoplastics in nearly 60% of them.
Crucially, patients with plastics in their arteries were 4.5 times more likely to suffer a heart attack, stroke, or death in the following 34 months compared to those who were plastic-free. These microscopic particles, inhaled from tires or ingested from food packaging, lodge in arterial walls, triggering constant, low-grade inflammation that accelerates clotting.
- The Noise Pollution Connection
- The Noise Pollution Connection
We often think of noise as an annoyance, not a killer. However, “Environmental Cardiology” has identified noise pollution as a potent vasoconstrictor. Chronic exposure to noise (road traffic, aircraft) over 50 decibels activates the amygdala—the brain’s fear center.
This triggers a cascade of stress hormones (cortisol and adrenaline) even while you sleep. This “fight or flight” response never turns off in urban environments, leading to stiffened blood vessels and hypertension. If you live near a major airport or highway, your risk of stroke is measurably higher, regardless of your diet.
- The Genetic Ghost: Lipoprotein(a)
While we obsess over LDL (bad cholesterol), a stickier, more dangerous particle called Lipoprotein(a) or Lp(a) often goes unchecked. Roughly 20% of the global population carries high levels of Lp(a) due to genetics.
Diet and exercise have almost zero effect on Lp(a). It acts like a Velcro strip for plaque, preventing clots from breaking down. For millions of “healthy” people who suffer sudden heart attacks in their 40s, untreated high Lp(a) is often the culprit. As of 2025, guidelines are finally shifting to recommend every adult be tested for Lp(a) at least once in their lifetime.
- The Gut-Heart Axis (TMAO)
Your steak dinner isn’t just affecting your cholesterol; it’s feeding your microbiome. When you eat red meat or eggs, gut bacteria digest the nutrients (choline and carnitine) and produce a compound converted by the liver into TMAO (Trimethylamine N-oxide).
High levels of TMAO suppress the body’s natural ability to flush out cholesterol and heighten the reactivity of platelets, making blood more prone to clotting. This establishes a direct link between gut health and heart attack risk, birthing a new field of “nano-functionalized probiotics” designed to starve these specific bacteria.
The Youth Crisis: No Longer an “Old Person’s Disease”
Perhaps the most alarming trend in the 2020s is the shifting demographic. CVD is aggressively migrating downward in age.
A 2025 AIIMS study on sudden deaths revealed a shocking statistic: over 50% of sudden deaths analyzed occurred in people under the age of 45. In the United States, heart attack rates for adults aged 35–54 have risen, especially among women.
Why? The convergence of “sitting is the new smoking” (sedentary jobs), ultra-processed foods, and extreme psychosocial stress. The “hustle culture” comes with a cardiovascular price tag. High-stress environments induce Takotsubo Cardiomyopathy (Broken Heart Syndrome), a temporary but dangerous weakening of the heart muscle, at rates never seen before.
The Global Disparity
Cardiovascular disease is also a lens through which we can view global inequality. While death rates have plateaued in wealthy nations due to advanced statins and surgery, they are skyrocketing in Low- and Middle-Income Countries (LMICs).
- 75% of CVD deaths now occur in LMICs.
- In these regions, rheumatic heart disease (caused by untreated strep throat) still kills children, while urbanization brings Western-style obesity and diabetes to populations genetically ill-equipped to handle high-sugar diets.
The Future of Defense: From Reaction to Prediction
The war against the “Silent Threat” is moving from the operating table to the algorithm.
- AI Cardiology: Artificial Intelligence can now predict cardiac risk using retinal scans (looking at the veins in the eye) or voice biomarkers (detecting subtle fluid buildup in the lungs via speech) long before a stethoscope can.
- The Polypill: A low-cost, once-daily pill combining a statin, blood pressure medication, and aspirin is being rolled out in developing nations, potentially cutting global CVD mortality by 20%.
- Gene Editing: For the first time, CRISPR-based therapies are entering trials to permanently switch off the genes responsible for high cholesterol and Lp(a), offering a “one-and-done” vaccine-style protection against heart attacks.
Conclusion
Cardiovascular disease remains the world’s leading disease not because we lack the knowledge to stop it, but because we have built a world that fuels it. From the microplastics in our water to the stress in our workplaces, modern life is inherently inflammatory.
Recognizing CVD as a “silent threat” requires a shift in mindset. It means looking beyond the scale and the cholesterol number. It means advocating for cleaner air, quieter cities, and food systems that nourish rather than inflame. Until we treat the environment and the lifestyle as the patient, the heart will continue to be the primary casualty of progress.
Quick Reference: The Hidden Risk Checklist
If you are over 30, ensure your next checkup includes:
- hs-CRP Test: To measure systemic inflammation.
- Lp(a) Test: A one-time genetic test for “sticky” cholesterol.
- ApoB Test: A more accurate predictor of risk than standard LDL.
- CAC Score: A CT scan to see if calcified plaque already exists.