The Most Outstanding MedTech Entrepreneur – 2025

Guillem Singla Buxarrais: Revolutionizing Neurorehabilitation with Technology, Transparency, and a Human-Centered Vision
By The Influential Today Magazine
In the rapidly advancing world of medical technology, true innovation is measured not only in sophisticated hardware or algorithms, but in the tangible, life-changing impact it has on patients. It is here, at the intersection of cutting-edge technology and profound human need, that Guillem Singla Buxarrais, Co-founder and Chief Executive Officer of Neurofenix, has distinguished himself as a leader of exceptional vision and purpose. The Influential Today Magazine is proud to honor Guillem Singla Buxarrais as The Most Outstanding MedTech Entrepreneur for 2025. His mission is not just professional; it is deeply personal. Through Neurofenix, he is pioneering a new era of telerehabilitation, dismantling long-standing barriers to care and offering hope for meaningful recovery to millions of neurological patients.
A Mission Forged in Family and Fueled by Science
For Guillem Singla Buxarrais, the drive to innovate in the field of neurorehabilitation is rooted in his own family’s experience. He witnessed firsthand the immense impact of neurological conditions in his own family. This personal connection to the struggle and the gaps in care became a powerful catalyst. He was not alone in this motivation; his co-founder, Dimitrios Athansiou, was similarly driven by his grandfather’s experience with stroke.
This deeply personal mission is supported by a robust academic foundation. A Biomedical Engineer by training, Guillem pursued a Master’s degree in Neurotechnology at the prestigious Imperial College London. His postgraduate work involved research into the complexities of the brain and behavior. It was the combination of seeing a “big gap” in available therapy services and having the scientific background to envision a solution that led to the creation of Neurofenix. He co-founded the company not just to build a business, but to address a fundamental need he understood with profound empathy.

A New Hope for Recovery: Addressing a Critical Gap in Care
The U.S. neuro-rehabilitation market presents an $18B+ total addressable opportunity, fueled by a growing demand for home-based therapy solutions across occupational, physical, speech & language, and cognitive domains. This surge is driven by an aging population and a nationwide shortage of therapists. With over 15 million Americans affected by common neurological conditions such as stroke, traumatic brain injury (TBI), spinal cord injury (SCI), brain tumors, Guillain-Barré syndrome (GBS), Parkinson’s disease, essential tremor, multiple sclerosis (MS), cerebral palsy (CP), and ALS, the need for scalable, accessible neuro-rehab has never been greater. At the same time, key trends—including value-based care, increasing payer reimbursement for remote therapy, the expansion of remote therapy monitoring (RTM), and the rise of AI-powered personalized rehabilitation programs and digital therapists—are reshaping how care is delivered and creating a unique window for innovation.
Stroke, in particular, remains a leading cause of long-term disability worldwide, with upper limb deficits affecting approximately 80% of survivors and severely limiting their independence and quality of life. Despite the high prevalence of these impairments, only about 12% of stroke survivors ever regain full function of their affected arm. The path to recovery is often fraught with challenges. Many patients, especially those with limited mobility or those living far from specialized facilities, face significant barriers to accessing the consistent, high-intensity therapy crucial for improvement. Transportation issues, the physical demands of travel, and a lack of resources often prevent survivors from participating in the very programs designed to help them.
It is this critical gap in the continuum of care that Neurofenix was created to fill. The company is revolutionizing neurorehabilitation by delivering comprehensive, high-dose, and high-intensity therapy directly to patients in their own homes. This innovative approach is particularly vital for patients for whom in-person outpatient therapy is not a viable option. By moving rehabilitation from the clinic to the living room, Neurofenix is not only improving accessibility but is also fostering the kind of consistent, daily engagement that is paramount for neurological recovery.

The Neurofenix Ecosystem: A Symphony of Technology and Personalized Therapy
At the heart of Neurofenix’s success is its unique and patented AI-powered rehabilitation technology, the NeuroPlatform™. This is not merely a single device but a comprehensive, integrated ecosystem designed to support every step of the patient’s journey. The platform was meticulously developed with input from over 600 clinicians and patients, ensuring it is both clinically robust and user-friendly.
Neurofenix’s virtual therapy programs typically lasts between 8 and 16 weeks and follow a structured, supportive pathway. Programs begin with a virtual evaluation by one of Neurofenix’s licensed neuro-rehab therapists, many of whom have over 20 years of experience. Based on this evaluation, a personalized Plan of Care is created, tailored to the patient’s specific condition and personal goals.
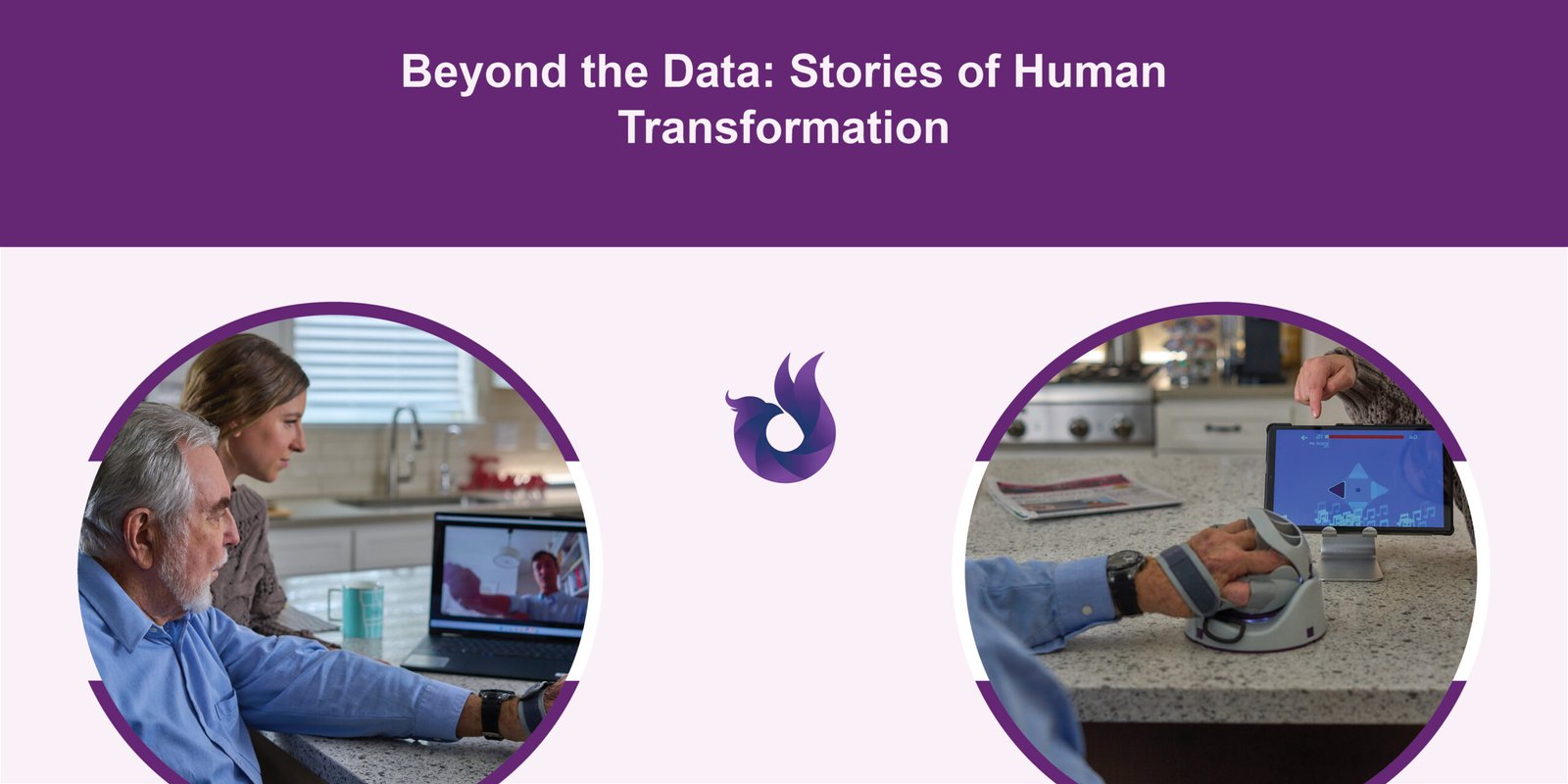
Following the evaluation, the patient receives Neurofenix’s Neuro Rehab Kit, which includes the company’s flagship product, the NeuroBall™. The NeuroBall™ is a sensor-based, FDA-approved medical device that integrates with a tablet to offer a wide variety of gamified therapeutic activities. This approach transforms what can be monotonous exercises into engaging and motivating challenges, encouraging the high number of repetitions needed for neuroplasticity.
Throughout the program, patients participate in weekly one-on-one therapy sessions with their therapist via video call. This is complemented by a home-based therapy plan that includes prescribed exercises on the NeuroBall platform and task-specific activities of daily living (ADLs). Crucially, the therapist remotely monitors the patient’s progress through the Clinician Dashboard, a custom-made web application. This allows them to track adherence, see real-time activity, and adjust the therapy plan as needed, ensuring continuous and personalized care. This multi-channel communication, including personalized messages, SMS, calls, and emails, keeps patients motivated and connected between sessions.
The Evidence of Impact: Clinically Validated, Data-Driven Results
What truly sets Neurofenix apart is its deep commitment to transparent, measurable, and clinically validated outcomes. The company’s approach is supported by four clinical trials, including an independent, non-sponsored study conducted by Brunel University of London and led by a leading specialist in upper extremity rehabilitation. Additionally, Johns Hopkins University conducted an independent clinical trial demonstrating significant improvements in patients’ function and overall independence. These trials have consistently demonstrated that the Neurofenix platform is feasible, safe, acceptable to patients, and highly effective.
The core principle behind the platform’s success is its ability to facilitate high-dose, high-intensity therapy. Research consistently shows that the number of movement repetitions is highly correlated with functional improvement. While a typical upper extremity therapy session may involve around 32 repetitions, the Neurofenix platform enables an average of over 656 repetitions per day, more than 20 times the conventional amount.
The results from numerous case studies are remarkable:
- Significant Functional Gains: Patients consistently show statistically significant clinical improvements across a range of validated measures. This includes the Stroke Impact Scale (SIS), where patients have seen scores improve by over 51.3% and 60%, and the Motor Activity Log (MAL), where improvements in the amount and quality of limb use have exceeded 300%.
- Improved Range of Motion (AROM): Objective measures show dramatic gains in joint mobility, with some movements improving by as much as 300% to 500%. In one study, 9 out of 9 AROM movements improved for the patient.
- Enhanced Independence: Patients have progressed on the Functional Upper Extremity Levels (FUEL) scale, moving from categories like “Gross Assist” or “Dependent” to “Semi-Functional” or even “Functional”. This represents a marked improvement in their ability to use their affected limb in practical, real-world tasks.
Since 2016, Neurofenix has collected over 26,000 hours of therapy, 31 million movement repetitions, and 680,000 therapy sessions from more than 3,000 patients – fueling their vision to deliver AI-powered personalized therapy that adapts to each patient’s unique needs.
Beyond the Data: Stories of Human Transformation
While the clinical data is compelling, the true measure of Neurofenix’s impact lies in the stories of the thousands of individuals whose lives have been transformed. Guillem often shares the story of Sally to illustrate the magic of their platform. Sally, a 65-year-old stroke survivor, struggled with basic tasks like eating and cutting food and faced a risk of falling. For Sally, traditional in-person rehab was impractical due to transportation challenges and her children being at work all day. After choosing Neurofenix, she quickly received a Neuro Rehab Kit at home, complete with a pre-set tablet, and began treatment with her virtual therapist, Katie, via video visits. The results were swift and life-changing. After just eight weeks, Sally could bring a spoon to her mouth, prepare a full meal by herself, and, most joyfully, she had returned to playing Connect4 with her grandchildren.
Consider Michael, a patient who was more than 20 years post-stroke. After 16 weeks with Neurofenix’s virtual rehab program, he was amazed by his progress. He saw increased movement in his fingers, was able to cut his own food and open containers, and could once again bait a fishing hook and go fishing. He regained the ability to walk with his arm extended naturally by his side. He was stunned, stating he “didn’t know he could do this much with his hand after 20+ years.”
Or Susan, who was three years post-stroke and highly motivated during her 16-week program. Her biggest goal was to be able to write again, and she achieved it, successfully handwriting paragraphs. She also regained the ability to perform a host of daily tasks, including making meals, cleaning her house, applying lipstick, and putting on her wig.
These are not isolated incidents. From Robert, who can now hold the steering wheel on his golf cart, to Don, who can now wash his hair and get dressed with less difficulty, the impact is consistently life-changing. One patient, Todd Johnson, summed it up powerfully: “I could not carry a garbage bag up to the garbage – I can do that now. I could not carry a shirt to the washer – I can do that now. I could not open a door – I can do that now.”

A Sustainable Model for the Future of Healthcare
Guillem Singla Buxarrais has built not only a clinically effective platform but also a sustainable and accessible business model. This has been achieved through strategic partnerships with many of the best minds and institutions in neurorehabilitation, including Spaulding Rehabilitation Network, Shirley Ryan AbilityLab, Johns Hopkins, NYU Langone Health, and Boston Children’s Hospital. These partnerships allow leading health systems to provide Neurofenix’s advanced technology to their own patients, extending their reach and ensuring continuity of care.
By combining cutting-edge technology with patient-centric therapeutic approaches, Guillem Singla Buxarrais and Neurofenix are setting a new standard for neurological recovery. Their work demonstrates that with the right tools, unwavering dedication, and a deep understanding of patient needs, and ongoing collaboration with clinicians, significant functional gains are possible, even for those many years post-neurological injury. He has created more than just a MedTech company; he has built a scalable and accessible solution that offers hope, restores independence, and profoundly improves the quality of life for neurological patients and their families around the world.